Andrew Priddy
Well-Known Member
Donator
Full Member
- Messages
- 1,561
- Reaction score
- 199
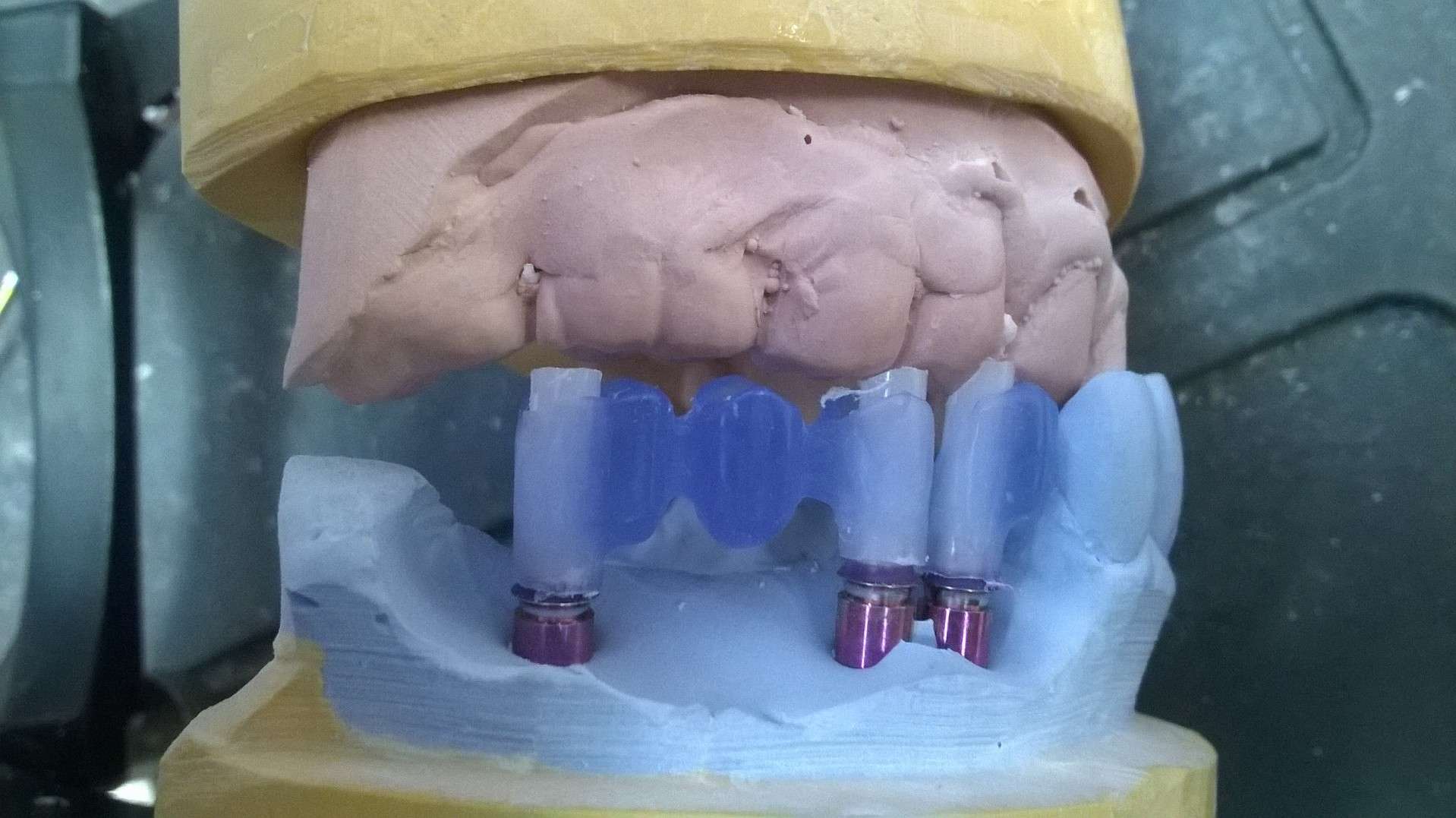
well, I wanted to try and design frames, mill in acrylic, and bond to cast-to's
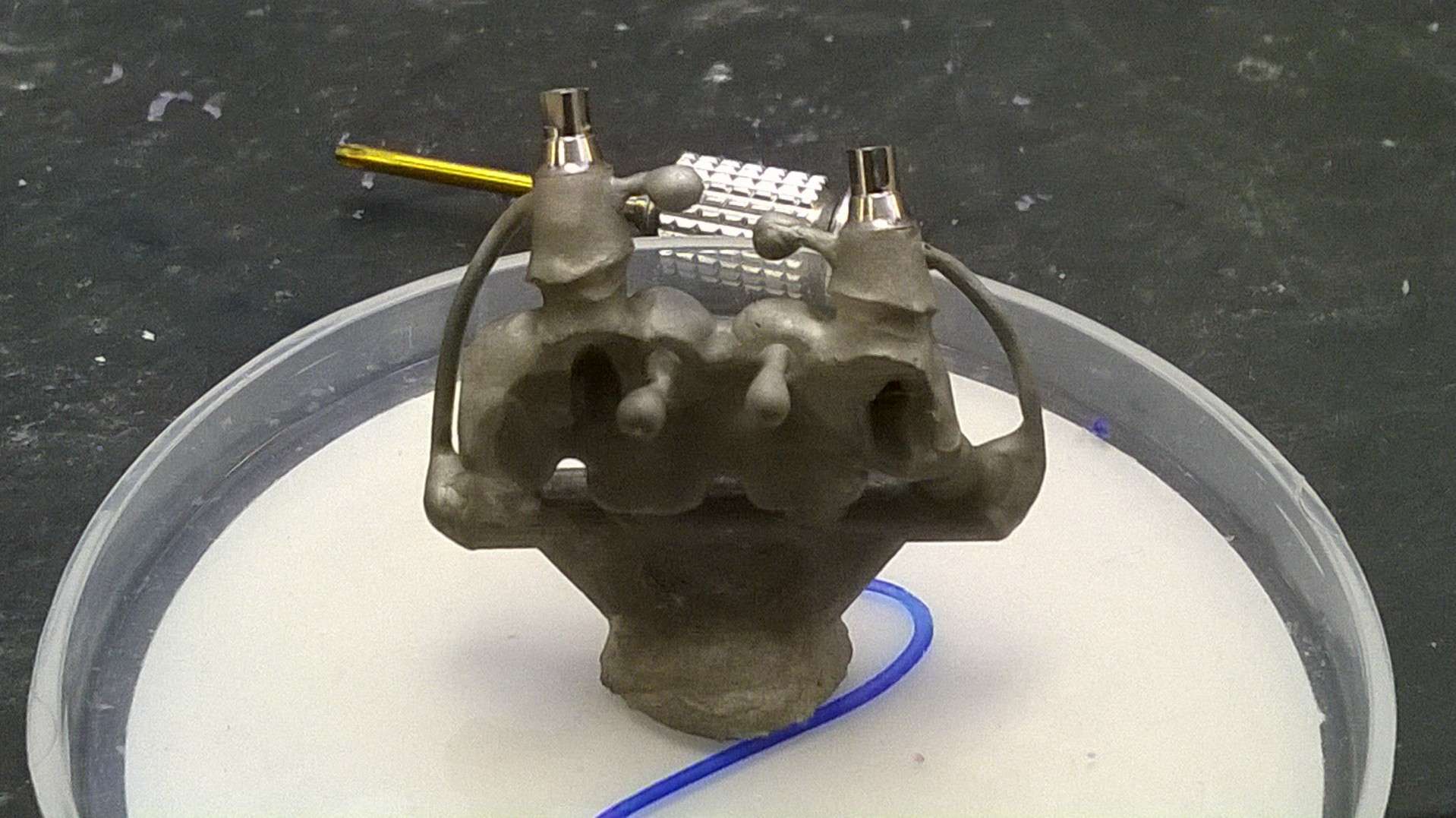
I set this up over tibases (vario)
i'm thinking Glidewell bases (setup) will work best for most platforms

don't worry about trying to design the cuff.. we will wax it in:
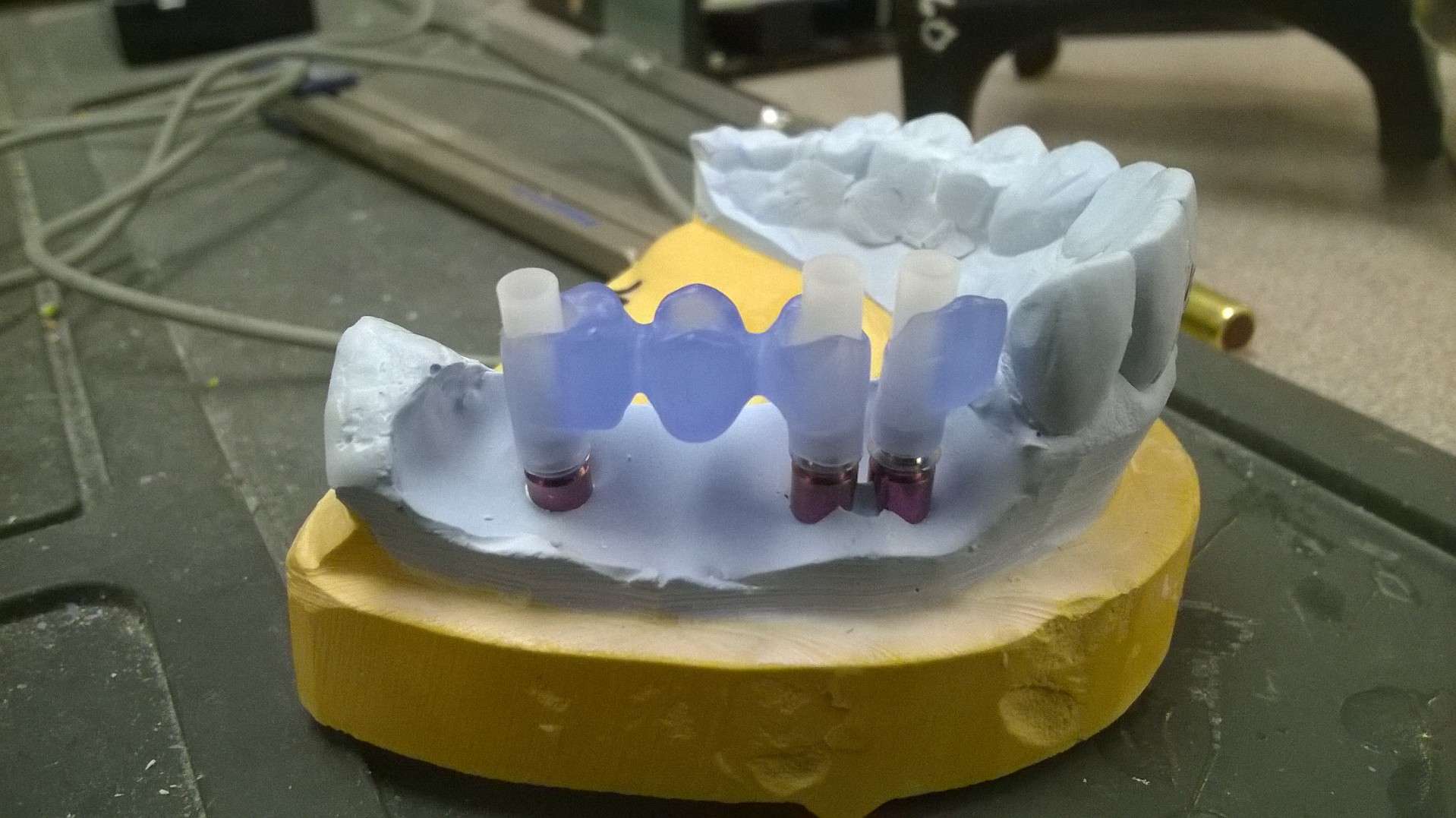
make sure the frame is very passive on multiple units.. don't be afraid to hog out the frame access holes.. you will need room the get acrylic to flow in
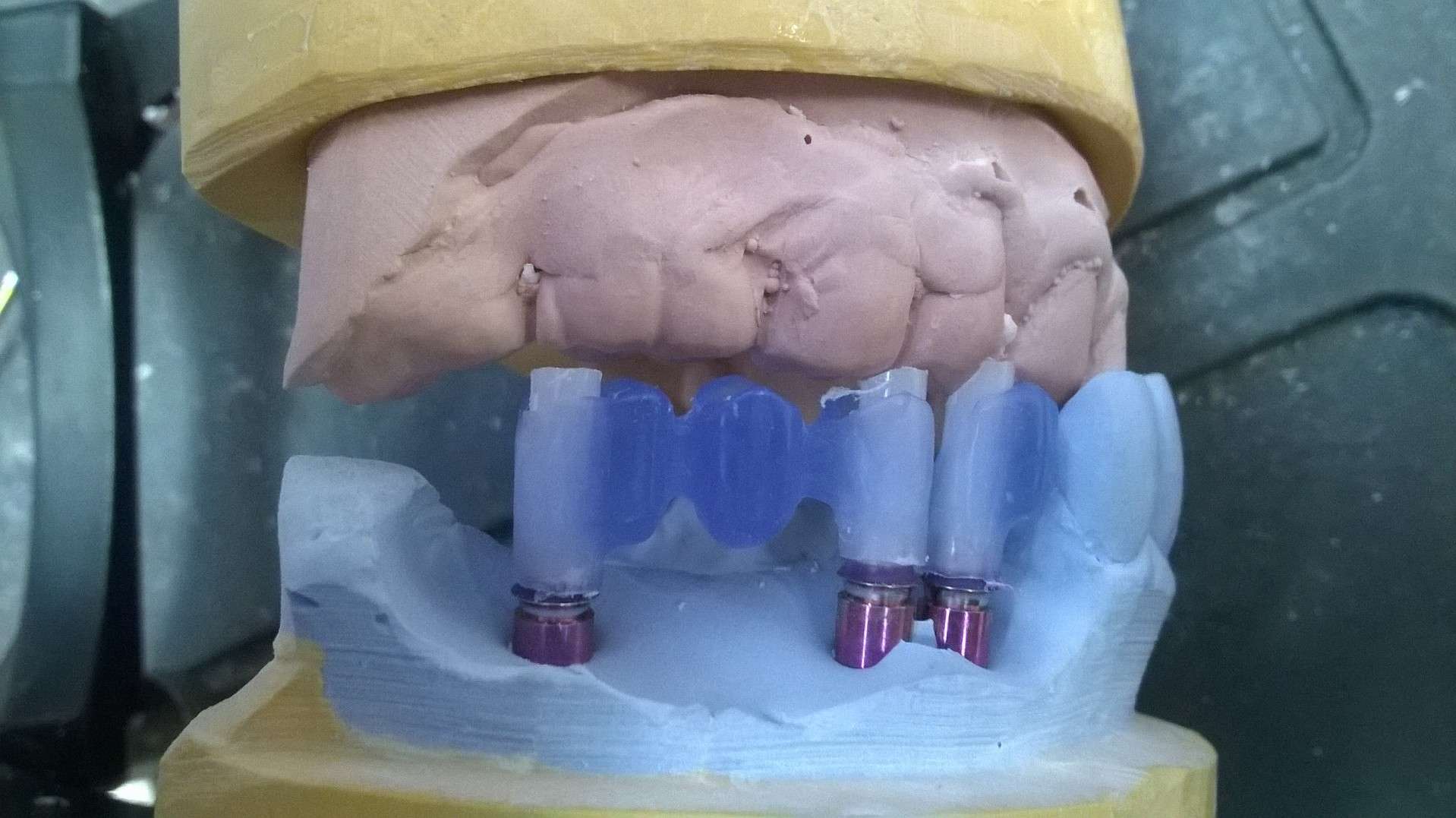
shave off some of the base of the frame and taper in the acrylic
cut the access tubes so you can adjust the frame to the occlusion.. also, I ran a wax bead around the UCLA at the cuff

seal the junction between frame and access tube at the bottom
fill the void between access tubes and frame with pattern resin/ picu-plast etc... notice that the access tubes are kept long to allow you to fill the void and not the screw access tube
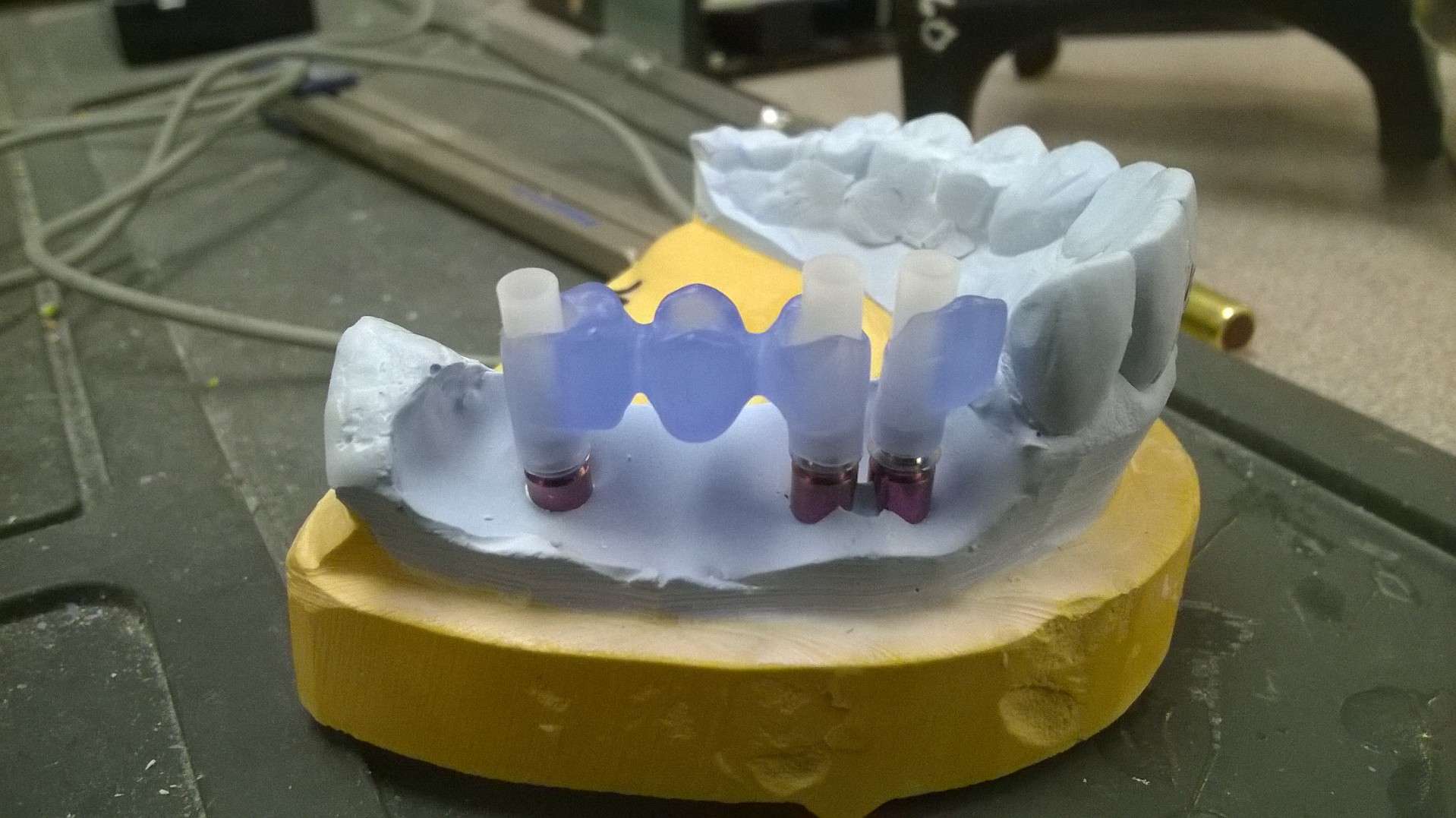
after the frame is stable, remove it.. sculpt the tissue, insert the frame, wax the cuff

clean up the access tubes, smooth the surface with wax, make any final adjustments

the frame is extremely stable
also, still using white-out without fail!
I set this up over tibases (vario)
i'm thinking Glidewell bases (setup) will work best for most platforms

don't worry about trying to design the cuff.. we will wax it in:
make sure the frame is very passive on multiple units.. don't be afraid to hog out the frame access holes.. you will need room the get acrylic to flow in
shave off some of the base of the frame and taper in the acrylic
cut the access tubes so you can adjust the frame to the occlusion.. also, I ran a wax bead around the UCLA at the cuff

seal the junction between frame and access tube at the bottom
fill the void between access tubes and frame with pattern resin/ picu-plast etc... notice that the access tubes are kept long to allow you to fill the void and not the screw access tube
after the frame is stable, remove it.. sculpt the tissue, insert the frame, wax the cuff

clean up the access tubes, smooth the surface with wax, make any final adjustments

the frame is extremely stable
also, still using white-out without fail!
Last edited: